Facilities strive to adhere to recommendations in guidelines and standards of practice to improve patient outcomes, yet guidance is often derived from highly-controlled clinical trials in select patients that are incredibly expensive to conduct and can take years to complete.
I have often wondered about the validity of those results in real world, day-to-day practice, especially as the need to improve practice often comes before new studies are published and guidelines are developed.
While the data derived from controlled studies are important to validate the efficacy of new technologies, is it realistic to expect effective and sustainable results when they are integrated into clinical practice?
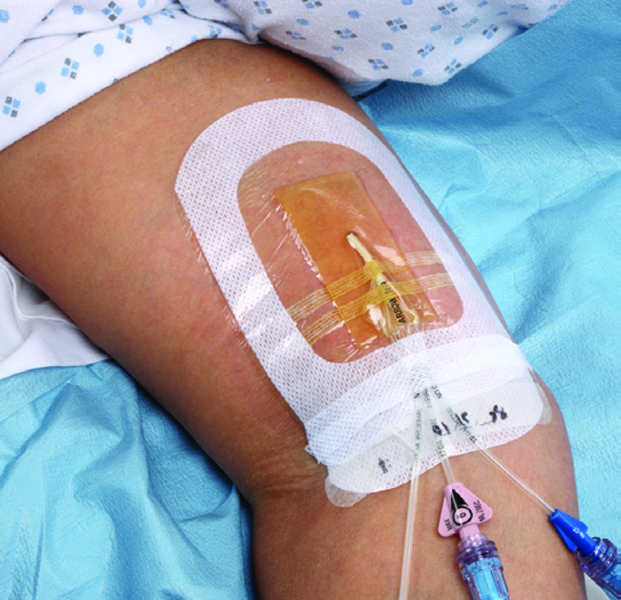
Findings from a new study* conducted by Eggimann, et al., examined the effect of adding chlorhexidine dressings to an existing catheter bundle of care in ICU patients. The study confirmed that clinical protocols derived from controlled trials can translate to sustainable improvements.
Among the highlights1:
Infection prevention measures recommended in the guidelines can be clinically effective in real world practice.
This study included over 18,000 critically ill patients and 155,000 catheter days and its real world design didn’t control for the realities of care delivery: complex, diverse patients, resource constraints and variable compliance to clinical protocols. The stepwise method used to refine the existing bundle is a realistic approach to practice improvement and resulted in a significant reduction in catheter-related bloodstream infections.
Sustained improvement over time is possible.
This study was conducted from 2006-2014 in which improvement of the infection rate continued over time. The low rate was further sustained over a four-year period after study completion.
Consistent training and feedback are essential.
Healthcare facilities are resource limited entities in which turnover is common and human factors inevitably affect protocol compliance over time. While compliance was not monitored in the study, systematic training and continuous feedback were provided which likely contributed to the sustained reduction in catheter-associated bloodstream infections over time.
Informing practice
As clinicians, we understand the importance of evidence-based practice and want to provide the highest standard of care for our patients. It is important to look to controlled studies to evaluate the efficacy of new interventions, yet it is also valuable to consider the application to daily clinical practice – the reality in which we work.
The Eggimann, et al., study provides value for clinical decision making because it confirms sustainable effectiveness of current recommendations with data collected under real world clinical circumstances.
To learn more, download a copy of the study here. Dr. Eggimann presented these findings on behalf of 3M at the International Conference on Prevention and Infection Control (ICPIC) in Geneva, on Sept. 12, 2019, and the Association for Vascular Access (AVA) conference on Sunday, Oct. 6, 2019, in Las Vegas.
* The study was partially supported by an unrestricted research grant from 3M.
References:
1. Eggimann P, Pagani J, Dupuis-Lozeron E, et al. Sustained reduction of catheter-associated bloodstream infections with enhancement of catheter bundle by chlorhexidine dressings over 11 years. Intensive Care Med. 2019; 45(6): 823-833. doi: 10.1007/s00134-019-05617-x
Like what you’ve read?
Consider subscribing to Transforming Outcomes to learn more about insights on skin, complications prevention and patient care.
