
Patient safety is always top of mind for hospitals and surgery centers. Delays in surgery during the initial months of the COVID-19 outbreak may mean a higher risk of complications for patients needing care. A backlog of patients and new safety protocols means managing efficiency is more important now than ever.
As patients and staff return to elective surgeries, there are new challenges, new safety concerns, and enhanced protocols.
Resources for safety
A top concern for both patients and staff is their safety and respiratory protection. Kim Prinsen, RN, MSN and clinical applications specialist for 3M Medical Solutions explains, “It is important to ensure your staff is comfortable with their selection of personal protective equipment (PPE) and they should know the proper donning and doffing procedures to protect themselves.” She says 3M has resources to help hospitals and surgery centers address safety concerns including information on choosing respiratory protection and optimizing the use of PPE.
3M also offers resources for infection prevention and cleaning monitoring based on WHO and CDC recommendations. Guidance for reducing contamination risks includes hand hygiene information, isolation room procedures and single-patient use considerations.
Operating efficiently
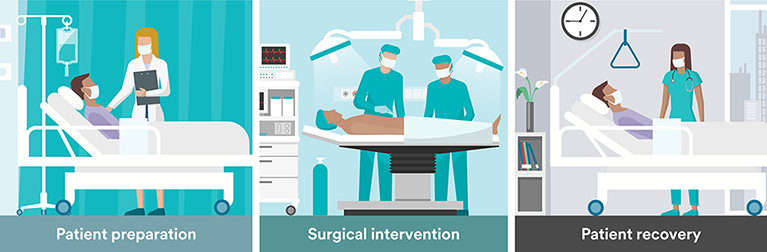
Kim adds that 3M has been having conversations with clinicians on an ongoing basis about how to optimize operating room time. With many surgery departments and surgery centers in varying stages of reopening, many are operating with a smaller capacity. Protocols may require that rooms remain vacant for a period of time between occupancy to allow time for air exchange and cleaning. That means the room time needs to be used optimally. “Patient flow in and out of the OR suite needs to be done safely and efficiently,” she explains, “and the surgical team needs to be ready to proceed once the patient arrives.”
Reducing complications
While the goal has always been for patients to move through surgery safely and begin the road to recovery without complications, the current COVID era has made clinicians look at the current process closely for additional steps that may help to reduce the risk of complications and reduce readmissions as much as possible.
There are methods to reduce the risk of complications by following evidence-based practices, applying consistent protocols, and defining what constitutes a high-risk patient and/or procedure today. “We are in an environment where we have always worked to reduce risk,” says Kim. “There are protocols we can follow for all patients, like patient temperature management and decolonization, that can further reduce risk.”
“Being focused on foundational practices is as important as always,” she says. “We take a lot of steps to get the skin ready and have a sterile incision. We also want to make sure the right product is chosen to protect the incision and have the best fit for the surgery location, the patient, and what is needed for their recovery.”
While the current environment is unique, Kim adds that patient safety is still top of mind. “Protocols and practices during the COVID-19 pandemic may change, and as we learn more, we adjust,” she says. “The things we have done and the steps we take to protect patients are still best practice.”
Protection throughout the patient journey
- Skin and Nasal Decolonization: 3M™ Skin and Nasal Antiseptic is a simple, one-time application that reduces nasal bacteria, including aureus by 99.5%, in just one hour and maintains this reduction for at least 12 hours.1 A recent article by Drs. Engelman and Arora recommends routine universal decontamination rather than nasal swabbing and screening urgent and emergent surgical patients for S. aureus to reduce the risk of exposure to healthcare workers posed by this practice. This is in addition to the CDC recommendations for nasal decolonization, at a minimum, for high risk surgical procedures.2,3
- Temperature Management: It’s important to maintain patients’ core temperature before, during and after surgery. Even a minor drop in core body temperature can result in unintended hypothermia, a common, yet preventable complication associated with an increased risk of surgical site infection (SSI), longer length of hospital stay, and other costly, potentially deadly consequences.4,5
- Antimicrobial Incise Drapes: You can help reduce the risk of surgical site contamination with antimicrobial incise drapes providing a sterile surface all the way to the incision edge and continuous broad-spectrum antimicrobial activity under the drape.
- Negative Pressure Wound Therapy: Economic models show that V.A.C. VERAFLO™ Therapy, compared to V.A.C.® Therapy, may help reduce the total cost of care for patients with infected or contaminated wounds through reduced length of hospital stay, trips to the OR, and length of therapy.6
- Incision Management: PREVENA™ Therapy aids in reducing the incidence of seroma and aids in reducing the incidence of superficial surgical site infections in Class I and Class II wounds.*
Learn more about clinically proven surgical solutions to protect you and your patients.
*PREVENA™ 125 and PREVENA PLUS™ 125 Therapy Units manage the environment of closed surgical incisions and remove fluid away from the surgical incision via the application of -125mmHg continuous negative pressure. When used with legally marketed compatible dressings, PREVENA™ 125 and PREVENA PLUS™ 125 Therapy Units are intended to aid in reducing the incidence of seroma and, in patients at high risk for post-operative infections, aid in reducing the incidence of superficial surgical site infection in Class I and Class II wounds.
Resources:
1 3M Study-05-011100.
2 Sievert DM, et al. Antimicrobial-Resistant Pathogens Associated with Healthcare-Associated Infections: Summary of Data Reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol 2013; 34(1):1-14.
3 Strategies to Prevent Hospital-onset Staphylococcus aureus Bloodstream Infections in Acute Care Facilities Website. https://www.cdc.gov/hai/prevent/staph-prevention-strategies Reviewed March 1, 2019. Accessed August 19,2019.
4 Kurz A, Sessler DI, et al. Perioperative Normothermia to Reduce the Incidence of Surgical-Wound Infection and Shorten Hospitalization. New Engl J Med. 1996;334:1209-1215.
5 Melling AC, Ali B, Scott EM, Leaper DJ. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. The Lancet. 2001 Sep 15;358(9285):876-80.
6 Gabriel A, et al. Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: clinical outcomes and potential cost-effectiveness. Eplasty 2014; 14:341.
