
“March 19, 2020 is a day I’ll never forget,” says Brittany, an ICU nurse in Phoenix, Arizona. “I started the day in my normal medical ICU unit, but that was the day we started to cohort all the COVID-19 patients into one unit.” Brittany was assigned to work in the COVID unit on that first day, but after that, it was optional. She has been volunteering there ever since March 19.
 Brittany has seen the impact on patients of all ages, including people much younger than she expected to see in the ICU. “We recently lost a 20-year-old,” she says. “All life is precious, but when you see someone who has barely started their life, it’s almost unbearable. There is a heavy emotional burden.”
Brittany has seen the impact on patients of all ages, including people much younger than she expected to see in the ICU. “We recently lost a 20-year-old,” she says. “All life is precious, but when you see someone who has barely started their life, it’s almost unbearable. There is a heavy emotional burden.”
Life has changed dramatically for Brittany, both inside and outside of work. She’s scared. She’s scared that even with the care she gives her patients, it won’t be enough. She’s scared for the health of herself and her husband.
 But most of all, she worries about her patients being alone. She sees their fear and she sees them dying without their loved ones. “We play music and we hold their hands,” she says. “We call their family but saying good-bye on a screen is just not the same as being with them in person.”
But most of all, she worries about her patients being alone. She sees their fear and she sees them dying without their loved ones. “We play music and we hold their hands,” she says. “We call their family but saying good-bye on a screen is just not the same as being with them in person.”
Bravery in the face of fear
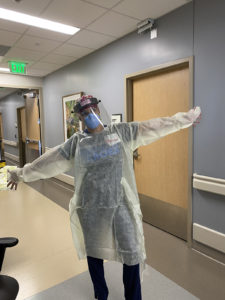 Brittney may be scared, but she is stronger and braver than even she realizes. Every day she shows up at work, walks in and fearlessly cares for her patients. Delivering that care has required significant change. The protocols for safety have changed dramatically. Every time a caregiver walks into a room with a patient who has, or potentially has, COVID-19, teams must don a gown, gloves, a scrub cap, safety glasses, an N95 respirator and a face shield. They also try to limit the number of people who enter the room and the number of times they enter. Clinicians try to cluster care into one visit instead of several visits to limit exposure and help save on PPE use.
Brittney may be scared, but she is stronger and braver than even she realizes. Every day she shows up at work, walks in and fearlessly cares for her patients. Delivering that care has required significant change. The protocols for safety have changed dramatically. Every time a caregiver walks into a room with a patient who has, or potentially has, COVID-19, teams must don a gown, gloves, a scrub cap, safety glasses, an N95 respirator and a face shield. They also try to limit the number of people who enter the room and the number of times they enter. Clinicians try to cluster care into one visit instead of several visits to limit exposure and help save on PPE use.
In the past when there was an emergency, the whole care team would rush into a room, but now they control who enters and they make sure they have on the appropriate personal protective equipment (PPE) before entering. “When I think that we ever walked around without a wearing a respirator, it seems unreal,” Brittany says.
Wearing PPE for extended periods is a new situation for most healthcare providers. Brittany and many of her peers wore an N95 respirator for patients with tuberculosis, but that was rare. “Now, we are usually wearing it for up to four days,” she says. “It makes me nervous, but at the same time it is helping provide the protection we need.”
 While acknowledging that wearing various PPE helps support their safety, Brittany says that wearing PPE for prolonged periods has contributed to her and many of her coworkers having acne, hives and/or other skin issues “It’s helping protect us, so we know it’s necessary through this period,” she adds.
While acknowledging that wearing various PPE helps support their safety, Brittany says that wearing PPE for prolonged periods has contributed to her and many of her coworkers having acne, hives and/or other skin issues “It’s helping protect us, so we know it’s necessary through this period,” she adds.
She has used powered air-purifying respirators (PAPRs) for aerosol generating procedures, when there are likely to be more virus particles in the air, like intubating patients to put them on ventilation. “It takes a lot of preparation to don the PAPR, but I find them more comfortable,” she says. Her administration recently announced that staff members could purchase and wear reusable respirators, so she is looking forward to trying one.

Strength in the future
While it’s been an emotionally draining time, Brittany appreciates her team and sees reasons to hope. She says she’s working with a group of people who wouldn’t have normally worked together in the past. “We have formed a new team with traveling nurses and people from other units and we really work great together,” she says. “We are always checking in with each other, even on days off. We need each other.”
“Sometimes, I wish people knew how much healthcare workers are sacrificing,” she adds. “Most of my coworkers haven’t seen many of their friends and family members for months. But we are willing to make these sacrifices – this is a pandemic and it’s what we are here to do.”
She also says she and her fellow nurses feel like they have a voice in making suggestions about what it is like working for patient care and they are being heard – their recommended changes have often been put into practice. “I hope we can continue to learn what works,” Brittany says. “As a country and as a people, I hope that we learn to help each other and protect each other.”
