
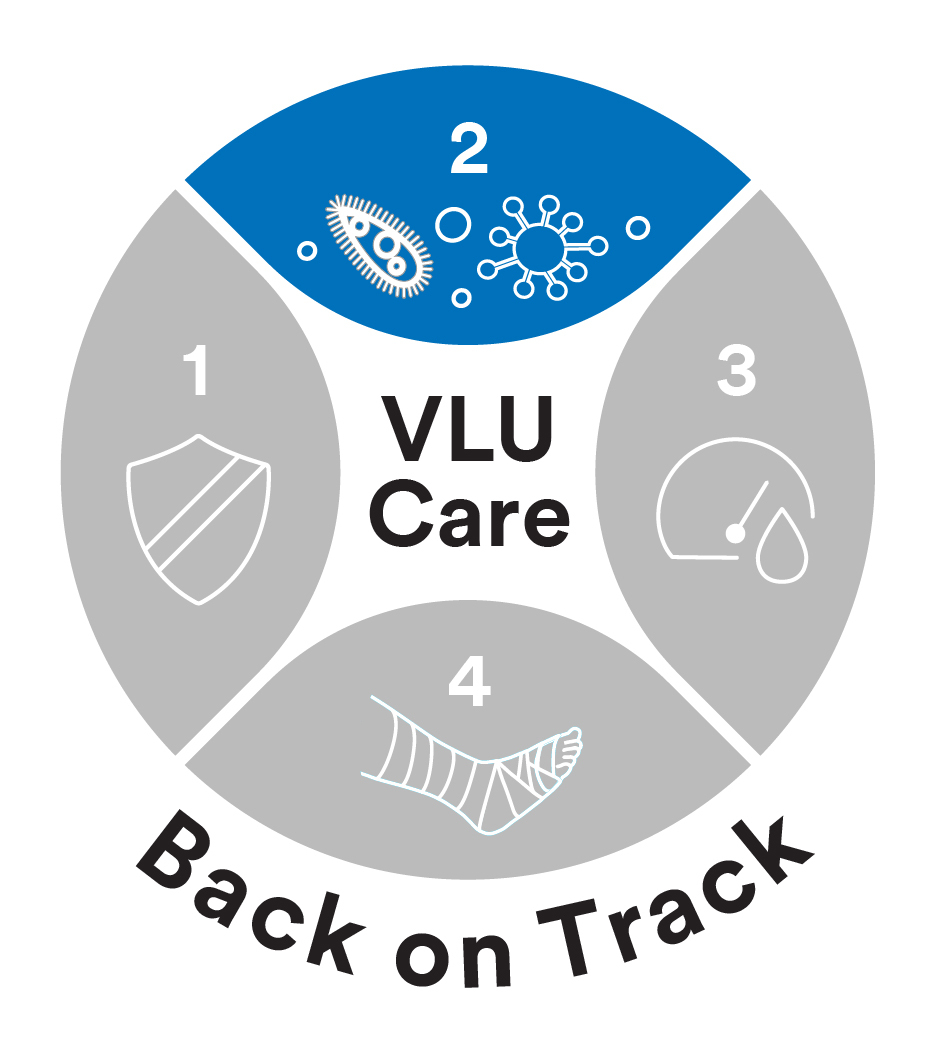
A graphical representation of biofilm.
The presence of biofilm complicates the healing trajectory of many chronic wounds including venous leg ulcers (VLUs). Joe Stoffel, a microbiologist who studies wound biofilm at 3M’s Medical Solutions Division, provides pertinent insight into the complexity of wound biofilm.
 For over 100 years, scientists like myself have studied bacteria, yeast, and other fungi in ideal laboratory conditions. This allows for controlled and meaningful experiments to develop and evaluate an antimicrobial product’s effectiveness. For example, when we want to show something can kill microbes, we grow a test tube of bacteria, drop in the antimicrobial and see if anyone survived. If all the bugs are dead, EUREKA! We’ve done it! Or have we?
For over 100 years, scientists like myself have studied bacteria, yeast, and other fungi in ideal laboratory conditions. This allows for controlled and meaningful experiments to develop and evaluate an antimicrobial product’s effectiveness. For example, when we want to show something can kill microbes, we grow a test tube of bacteria, drop in the antimicrobial and see if anyone survived. If all the bugs are dead, EUREKA! We’ve done it! Or have we?
This is how the FDA guides us to perform the test, but it only shows the product can kill planktonic bacteria.
What are planktonic bacteria? Planktonic literally means free floating, like plankton in the ocean.
In this state, bacterial cells are easily exposed to our antimicrobial, and there are few to no barriers standing in the way. Our chances of success are pretty good. So… what’s the problem?
We don’t live in the ocean or find ourselves routinely suspended in liquid. The microorganisms that live on us or infect our tissues aren’t either. A microbe’s preferred lifestyle is to attach to surfaces: on rocks in a stream, the ring that forms in our showers and toilets, and yes, that film on our teeth when we wake up in the morning. These are all examples of what we call biofilm.
How does biofilm occur?
Once microbes settle on a surface, they will immediately begin building a house. Microbes secrete a protective slime layer called the extra-polymeric substance, or EPS, in which they encase themselves. This does not occur when organisms are planktonic. The EPS allows the microbes to become increasingly tolerant to any changes in their surroundings, and routinely contains several different species of microorganisms within the same biofilm. The cells within the biofilm can also have an altered metabolic state or “hibernate”. In addition to the physical protection the EPS has provided, this hibernation state is another way these cells withstand external assaults such as topical antimicrobials.
Biofilm impact on wound care
Managing biofilms must be a consideration when creating a treatment plan for chronic wounds. Studies by James et. al1 and Johani2 et. al have shown that microbial biofilms can be found in nearly every non healing wound, and their presence can trigger chronic inflammation. Although clinicians are not necessarily able to visualize biofilm itself, evidence of a biofilm complicating healing may present as wounds make progress but then suddenly stall or regress. When treating a wound where biofilm is suspected, clinicians often reach for topical antimicrobials in addition to other interventions, including debridement. However, every FDA cleared antimicrobial product has achieved its antimicrobial status by testing against planktonic organisms, those free-floating versions of microbes that you are unlikely to encounter when treating real wounds. One may ask, “why aren’t products tested against biofilms?” The answer is complicated.
There are several biofilm models for testing wound care products published in literature, but none are standardized. A product may perform very well in model A, but then be completely ineffective in model B. Without standardization, the testing conditions in model B may be altered to produce the desired result. This makes comparing results between products nearly impossible.
Biofilms in chronic wounds are a real problem and should be considered. Creating an effective management plan specific to biofilm based wound care based on consensus documents3 is key. Finally, deciphering the facts around antimicrobial product claims is essential to achieving appropriate data driven decisions. To help do so, learn more about biofilm testing models in a recent The Journal of Wound Repair and Regeneration article.
References:
1 James et.al. Wound Rep Regen. DOI:10.1111/j.1524-475X.2007.00321.x
2 Johani et. al. Int Wound J 2017; DOI:10.1111/iwj.12777
3 Snyder RJ, Bohn G, Hanft J, et al. Wound Biofilm: Current Perspectives and Strategies on Biofilm Disruption and Treatments. Wounds. 2017;29(6):S1-S17.
