Patient experience and patient journey are two terms used in healthcare, often interchangeably, to describe how we thoughtfully interact with patients. However, these two terms refer to very different aspects of patient care. While most clinicians enter the patient’s journey for a moment in time, adding to the experiences that become their overall journey to wellness, there are few roles that allow the nurse to experience the full journey with the patient.
I learned, in one of those roles, that having a holistic view of the patient journey can make all the difference.
As a renal and pancreas transplant coordinator, I was the core touchpoint for all my patients. It was common to care for over 1,000 patients simultaneously, as when you receive an organ transplant the coordinator becomes like a member of your family, often for life. From the point of transplant, I constantly worked to ensure the patient could get labs drawn, reviewing those labs for trends or abnormalities and ensuring they were able to receive their medications without pause and took them correctly. In our complex health care system, doing all this could sometimes mean moving mountains to ensure patients have what they need. This close relationship helps ensure care is done holistically, with the patient at the core of the decision-making process. Eventually, recipients become less dependent on their coordinator, yet will reach out for every medical ailment or question, no matter how unrelated to their transplant it may be.
By closely following the patient journey, the coordinator can pick up on nuances that, ultimately, can be lifesaving. And, for Ron* that was literally the case. Ron was a new renal transplant recipient challenged with a lack of healthcare knowledge and support system as well as extreme comorbidities. Like many patients, I worked with him very closely following his transplant, and I learned that he loved coming into the clinic to learn about his health and how he could continue to improve to become more independent in his care. He enjoyed talking with all the coordinators, nephrologists, and surgeons and looked forward to his appointments. One day, he didn’t show up and when I called, he didn’t answer. Sixty minutes went by and still nothing. Most would leave it at that, with a voicemail to reschedule the appointment. But I knew that while Ron had many challenges, he was dedicated to his health care. When there was no answer from his emergency contact as well, I called 911 for a welfare check.
Ron was found unconscious. He had fallen in the middle of the night and couldn’t get up. He was transported to the hospital where he spent several days and, while he had a serious wound from his fall, he ultimately recovered.
While not all stories will involve literally saving someone’s life, Ron’s story is just one example of the difference a health care advocate following along the patient journey can have on the patient’s experience and outcomes.
Just a few additional ways this style of care can save both resources and money for the facility and patient may include:
- Ensuring the patient does not undergo unnecessary procedures. When we know a patient already had a procedure done, even if in another health system, we can navigate the system to receive the results and reduce extra work.
- Reducing the number of physician visits. The patient can talk to their transplant coordinator about any medical concerns and we can provide them direct access to the correct specialty clinic rather than numerous physician visits to address an issue.
- Faster therapeutic care. When a patient is prescribed a medication they previously reacted poorly to, we can call their physician to have them try something else.
Navigating the complex health care system is never easy, and I often consider how many patients could be helped and how many lives could be saved if they had a health care advocate such as a transplant coordinator. Understanding the full patient journey is key to improving the patience experience and ultimately improving outcomes. Most clinicians enter the patient’s journey for a moment in time, yet when we can put those experiences together, we can support the patient on their journey and provide holistic care that is empowering and effective.
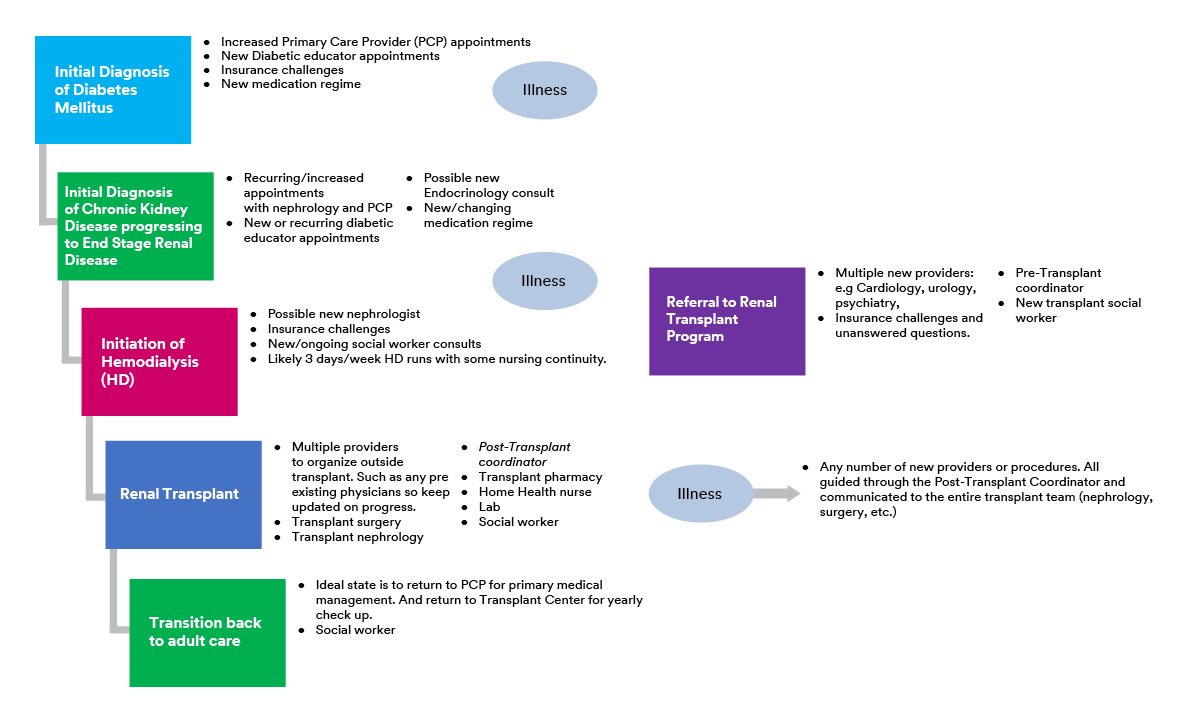
This example of a transplant patient’s experience through the health care system shows how complex and challenging the patient journey can be, with many touchpoints involving various different care providers.
*Name has been changed.