We know fecal incontinence and diarrhea are everyday problems in critical care; however, they can be found in all healthcare settings, and exposure to liquid stool, particularly when mixed with urine, is a significant risk factor for incontinence associated dermatitis (IAD). We also know that IAD increases the risk of secondary infection and is painful for patients. But, perhaps less commonly known is that IAD has been shown to be an independent risk factor for pressure injuries (PIS) 1-3.
Improving IAD prevention efforts could help address the growing issue of pressure injuries; understanding how to do so requires knowing how IAD and pressure injuries are connected.
Exposure to wetness – from urine and liquid stool – decreases skin strength, compromises barrier function, and makes skin more susceptible to damage from friction. Friction not only contributes to IAD, but it is also necessary for shear force.
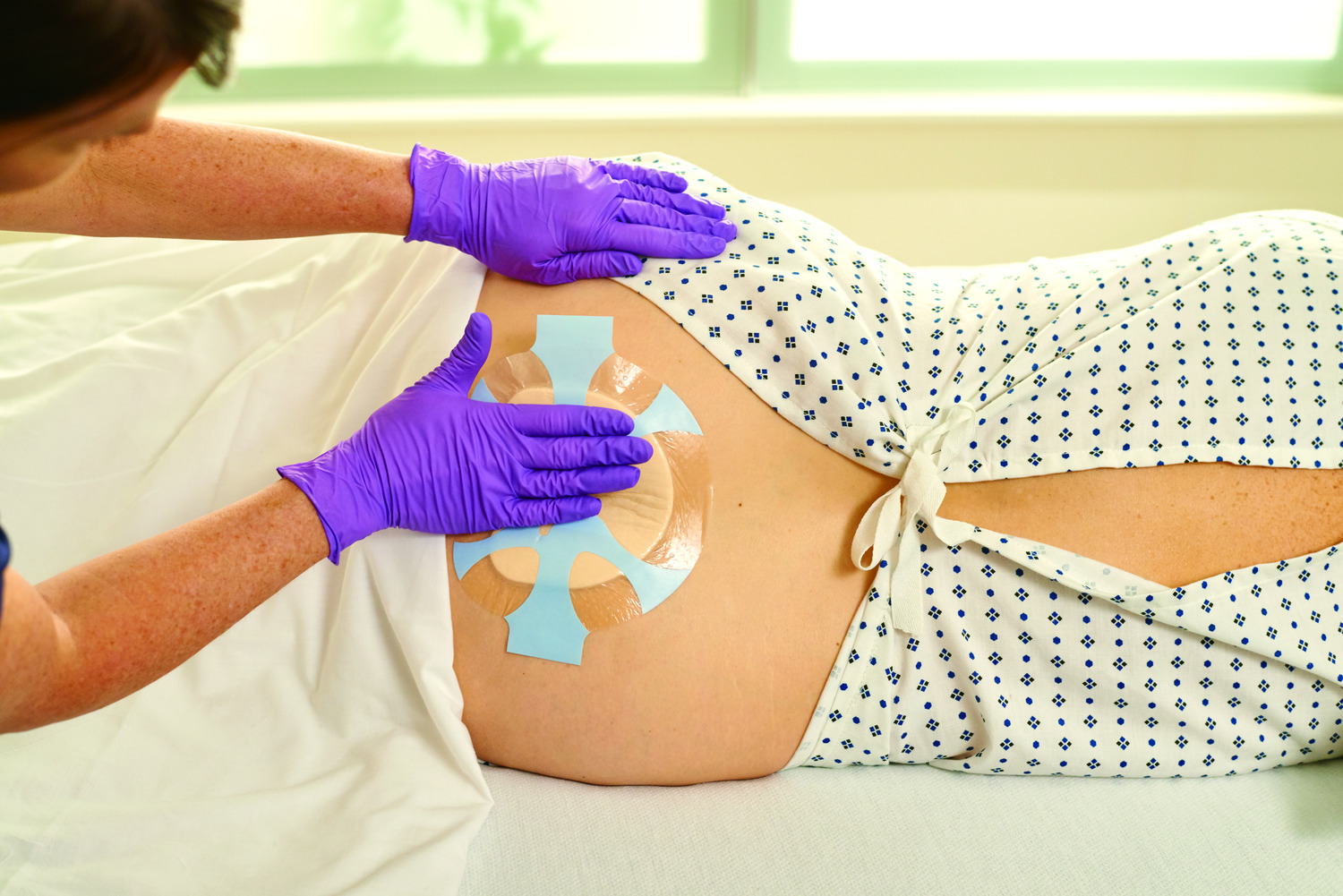
As a key component of pressure injury prevention, you are likely already using a variety of strategies to reduce friction such as low friction support surfaces, minimizing layers under the patient and/or protecting vulnerable areas with coatings or dressings. Another area to consider? Your moisture barrier ointment or paste. Recent laboratory data has shown us that some traditional moisture barriers used for preventive skin care can increase friction4.
With the potential impact of shear strain on pressure injury development, take a closer look at your IAD prevention methods and ensure they do not increase friction but rather help reduce risks that contribute to pressure injuries.
References:
1. Demarre L, Verhaeghe S, Van Hecke A, Clays E, Grypdonck M, Beeckman D. Factors predicting the development of pressure ulcers in an at-risk population who receive standardized preventive care: secondary analyses of a multicentre randomised controlled trial. J Adv Nurs. 2015 Feb;71(2):391-403.
2.Park KH. The effect of a silicone border foam dressing for prevention of pressure ulcers and incontinence-associated dermatitis in intensive care unit patients. J Wound, Ostomy, Continence Nurs. 2014; 41(5):424-29
3. Gray M, Juliano KK. Incontinence-Associated Dermatitis, Characteristics and Relationship to Pressure Injury: A Multisite Epidemiologic Analysis J Wound Ostomy Continence Nurs 2018; 45(1): 63-67.
4. Zaratkiewicz, S., Whitney, J. D., Lowe, J. R., Taylor, S., O’Donnell, F., & Minton-Foltz, P. (2010). Development and Implementation of a Hospital-Acquired Pressure
5. Declines in Hospital-Acquired Conditions. Content last reviewed May 2019. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/data/infographics/hac-rates_2019.html.
Ulcer Incidence Tracking System and Algorithm. Journal for Healthcare Quality, 32(6), 44-51.
6. Asmus R, Bodkhe R, Ekholm B, Thayer D, and Bradley J. The Effect of a High Endurance Polymeric Skin Protectant on Friction and Shear Stress. Poster presentation at 2018 Symposium on Advanced Wound Care Las Vegas NV and 2019 National Pressure Ulcer Advisory Panel Annual Conference St Louis MO.
7. Grove G, Houser T, Grigoryan A, Damia J. Atwood N. A motorized sliding sled for measuring the coefficient of friction of human skin in vivo. Poster presentation at 2011 Symposium on Advanced Wound Care. Dallas TX, 2011 European Wound Management Association Conference. Brussels BE, and the 2011 Wound Ostomy and Continence Nursing Society Conference New Orleans LA.
